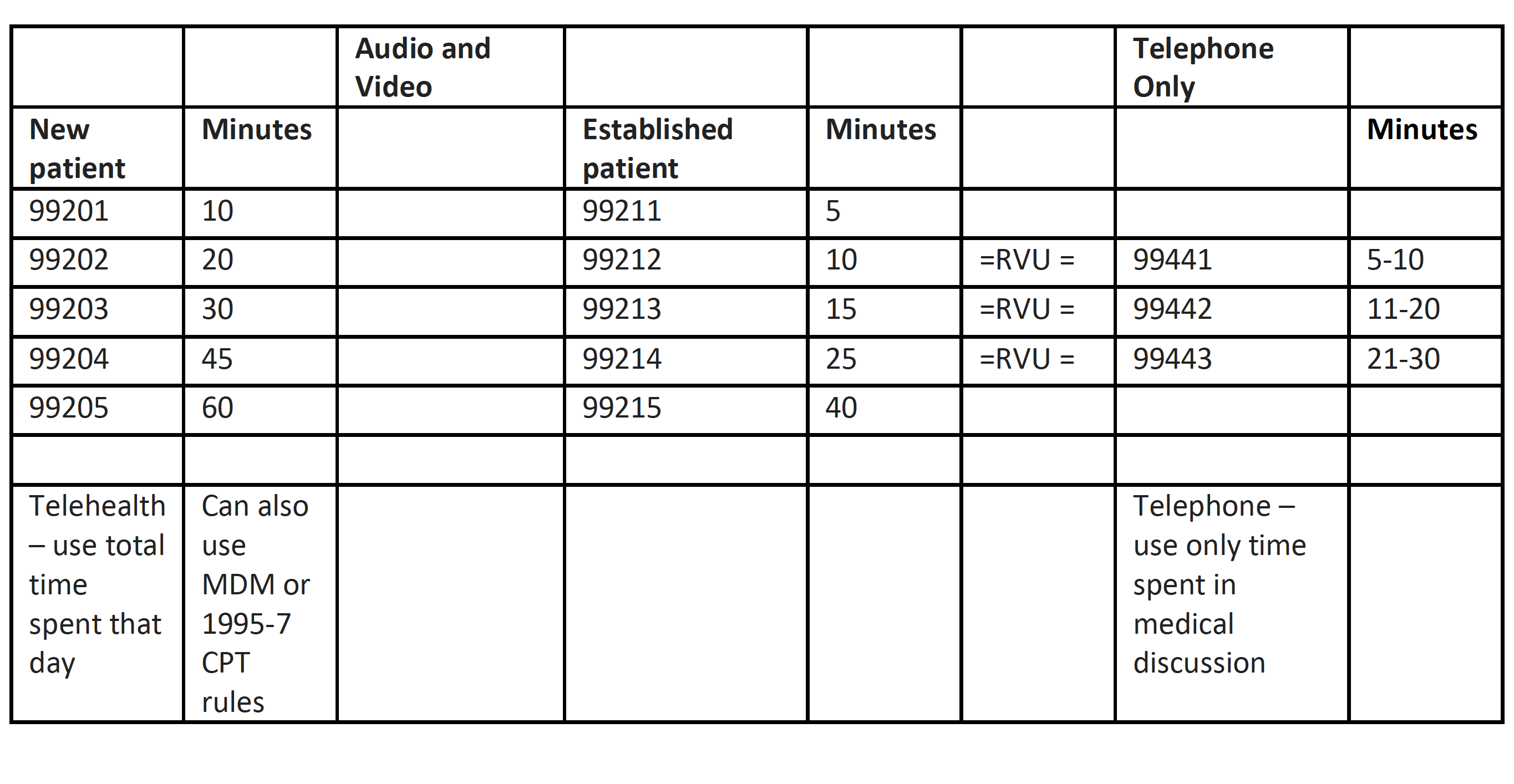
COVID-19 Regulatory Update – 5/2/2020May 2, 2020 Summary of Key Portions of New CMS Waivers Released April 30, 2020 Ronald Hirsch, MD, CHCQM, FABQAURP Telehealth – The Centers for Medicare and Medicaid Services (CMS) are allowing therapists to provide their services via telehealth. Prior to this, they were excluded from billing their traditional therapy codes as they were not allowed to bill by regulation. This means that these therapists who are employed either by a hospital, clinic, or independent may provider therapy services via FaceTime, Zoom, or other modalities and their services billed as if they were performed in person. The claims would be billed with the place of service as if the patient was seen in person with the -95 modifier added to the claim. This allowance is retroactive to March 1st so if therapy telehealth therapy services have been provided prior to April 30th, they may be billed. For physician visits with patients, CMS had previously approved the telephone billing codes 99441-99443 for payment but in this rule, they assigned these codes RVUs equal to mid-range established patient office visits performed via telehealth. Both the telephone and telehealth (audio and visual) codes can be chosen based on time but as noted in the table below, the methods for counting time vary. If your physicians are billing these codes, be sure they record time spent in the note.
Provider-Based Clinics – CMS is allowing facility fee billing for employed physicians who normally bill using place of service 19 or 22 for their office visits and who are performing telehealth visits with patients. In order to do this, the hospital must designate the patient’s home as a temporary provider-based facility. To do that, the hospital submits an extraordinary relocation exception request to their CMS Regional Office within 120 days of starting to bill for such services. According to the Rule, a single request can be submitted to designate every patient’s home as a provider-based facility and as long as the patient is registered as an outpatient for the service they are receiving, or have received. In this case, the physician would continue to bill their visit and add modifier -95 and the hospital would submit the originating facility fee Q3014. This same provision may also be used to allow provision and billing of services normally provided on the hospital campus by clinical staff such as wound care, chemotherapy administration, and other drug administration that are ordered by a physician and administered incident to that order with general supervision. In this case, the hospital could provide infusion services in a rented space, a hotel, a tent, or even rent space in a physician’s office (at above market value with the Stark Law waivers) and provide services there. CMS is also allowing billing of services provided by clinical staff to patients at home via telehealth for outpatient therapy such as psychotherapy, counseling, and educational services which are ordered by a physician and provided incident to that order with general supervision. It is worth noting that CMS did clarify on a recent call that when telehealth visits are conducted, the patient must continue to be assessed for updated insurance information and must be asked the usual Medicare Secondary Payer questions. On the other hand, the patient does not have to give formal consent to allowing the telehealth visit to be billed to Medicare as is required for the pre-waiver approved telehealth visits such as virtual check-ins and chronic care management. Free-Standing IRFs – CMS is allowing free-standing Inpatient Rehabilitation Facilities (IRFs) to admit patients who do not need IRF care but require ongoing inpatient care if it is specifically done to provide surge capacity for an acute care hospital as defined by the federal guidelines. This might be done to move non-COVID-19 patients who continue to require inpatient care and whose care can be adequately provided in an IRF to the IRF to open a bed for a COVID-19 patient. IMM/MOON – May 1st was the deadline for starting to use the updated Important Message from Medicare (IMM) and Detailed Notice of Discharge (DND), and the old Medicare Outpatient Observation Notice (MOON) with a new expiration date. I did request a delay beyond May 1st, and they did acknowledge my request, but it was not fulfilled. As a reminder, if you use an out-of-date form, you may be cited by a surveying organization and the patient cannot be held liable for any financial obligations that were addressed in the form but you may still bill for the service provided and you will get paid. If you have not updated your forms and you are in the midst of a COVID-19 surge, ask your compliance officer to carefully document the circumstances and the plan to implement the new forms as soon as feasible. |